Prostate Cancer
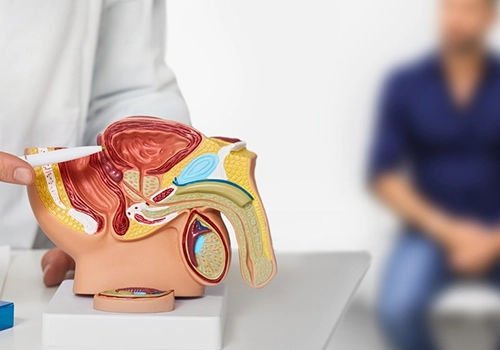
The prostate is a small, walnut-sized gland in the male reproductive system responsible for producing semen and providing nourishment and protection to sperm. The urethra, which carries urine from the bladder out of the body, passes through the central part of the prostate. Prostate gland diseases are common among men and often result from the uncontrolled proliferation of prostate gland cells.
In light of prostate cancer, it is crucial to understand that the manifestation of related symptoms does not necessarily imply the presence of cancer. Readers must grasp that examinations performed by non-specialists should not induce fear or anxiety.
It is essential to acknowledge that medical advancements worldwide have significantly increased the likelihood of successful treatment for various types of cancer. Therefore, taking timely actions to facilitate treatment is of utmost importance.
What is Prostate Cancer
As men age, the size of the prostate gland increases, which can lead to benign prostatic hyperplasia (BPH) or prostate cancer. Consequently, the risk of prostate cancer rises with age.
Specific forms of prostate cancer are classified as non-invasive, thus lacking noticeable symptoms in affected individuals. On the other hand, advanced prostate cancer often exhibits symptoms that are significant for the patient.
Typical symptoms associated with prostate cancer in men include urinary issues, sexual dysfunction, discomfort, and numbness.
The signs of prostate cancer
- Urinary Problems
Urinary problems are a common sign of prostate cancer. Since the prostate gland is situated near the base of the bladder, a tumor growing there may affect the bladder or the urinary tract, ultimately leading to problems. Urinary-related conditions may include:
- Frequent urination
- Slower urinary flow than usual
- Blood in the urine (hematuria)
- Sexual Problems
Erectile dysfunction, often referred to as sexual impotence, can be an indicator of prostate cancer. This condition deprives the individual of the ability to achieve and maintain erections. Additionally, blood in the ejaculate may also be indicative of this type of cancer.

Metastatic or advanced cancer is characterized by the migration of cancer cells from their primary site to distinct areas of the body. When Prostate cancer becomes metastatic, often spreads to the bones, causing discomfort in various regions including:
- Pelvic region
- Lower back
- Chest area
If cancer spreads to the spine, an individual may experience loss of sensation in both lower limbs and may also experience bladder dysfunction.
Warning Signs of Prostate Cancer
While prostate cancer can manifest through various symptoms, urinary symptoms typically appear among the first signs. Nevertheless, it is essential to acknowledge that many non-cancerous conditions such as benign prostatic hyperplasia (BPH) and prostatitis (inflammation of the prostate) can also create similar symptoms.
Consequently, vigilant monitoring of any warning signs is crucial, but it is also possible that these symptoms may not necessarily be cancer-related.
Causes of Prostate Cancer
There is a wealth of scientific research on a global scale that identifies the genetic roots of prostate cancer. Specific risk factors have been discovered in this field, and a widely accepted consensus currently assumes that:
- Obesity or metabolic syndrome
- Sedentary lifestyle and lack of exercise
- Excessive consumption of dairy or protein
- Overactive sexual behavior
- Family history of cancer, especially if a father, brother, or second-degree relative was affected
- Aging
Types of Prostate Cancer
- Benign Prostate Hyperplasia (BPH)
With advancing age, the prostate gland undergoes a process of enlargement, commonly known as benign prostate hyperplasia (BPH). This process subsequently leads to the development of malignant changes in prostate gland cells, referred to as prostate cancer. Therefore, it is essential to note that benign prostate hyperplasia is not prostate cancer.
- Malignant Prostate Cancer
There are two distinct types of malignant prostate cancer:
- The first type of malignant prostate cancer is associated with high PSA levels and a high degree of malignancy. However, it remains localized within the prostate gland, allowing for a natural lifespan if surgical intervention or radiation therapy is pursued.
- The second type represents a more aggressive form of malignancy that has progressed beyond the confines of the prostate gland and has affected lymph nodes, the liver, lungs, and bones.

Prostate Cancer in Younger Individuals
- In theory, all men have the potential to develop prostate cancer, with its prevalence increasing with age.
- The likelihood of prostate cancer in individuals under 39 years of age is 1 in 10,000. For those between 40-59 years old, this likelihood increases to 1 in 100, and in the age group of 60-79, it becomes 1 in 8.
- Every decade after the age of 40, the risk of prostate cancer doubles. The chance of developing prostate cancer at the age of 50 is 10%, while at 80 years old, it rises to 40%.
- For individuals with a family history of prostate cancer, the risk of developing the disease increases fivefold.
Risk of Mortality in Prostate Cancer
If prostate cancer is detected in its early stages when it is confined to the prostate, it does not carry a risk of mortality. With surgical or radiation therapy treatment, individuals can have a 95% chance of achieving a normal lifespan. However, if diagnosed late, when cancer has spread beyond the prostate and affected lymph nodes, bones, the liver, or lungs, the expected lifespan with hormone therapy treatment will be approximately two years.
Diagnosing Prostate Cancer
Screening for prostate cancer is often based on personal preferences. According to the Centers for Disease Control and Prevention (CDC), this is primarily because prostate cancers often grow slowly and pose little immediate threat to a person’s health.
Additionally, the results of the prostate-specific antigen (PSA) test, which can be part of the screening, may lead to false-positive diagnoses. For these reasons, screening can lead to unnecessary concern and unnecessary treatment.
Prostate Cancer Screening
The cancer community recommends specific guidelines for prostate cancer screening in conjunction with aging in men. It is recommended that during an annual check-up, doctors discuss the benefits and drawbacks of prostate cancer screening with men in specific age groups. Here are the recommended age groups:
- Age 40: Men at high risk of prostate cancer are advised to consider screening. This applies to individuals with a first-degree relative (father, brother, or son) who was diagnosed with prostate cancer before the age of 65.
- Age 45: Men at higher risk, such as African-American men and those with a first-degree relative diagnosed with prostate cancer before the age of 65, should consider screening.
- Age 50: Men at average risk of developing prostate cancer are recommended to consider screening. These are men who are expected to live at least another 10 years.

Prostate Cancer Diagnosis
When a person and their physician consider prostate cancer screening appropriate, the doctor will likely conduct a physical examination and discuss the patient’s health history. Additionally, physicians may perform various tests, including:
- Digital Rectal Examination (DRE)
- Prostate-Specific Antigen (PSA) Test: This blood test measures the level of PSA, a protein produced by the prostate gland.
- Prostate Biopsy: If necessary, a doctor may recommend a prostate biopsy to confirm the diagnosis of prostate cancer. During a biopsy, a small piece of the prostate gland is sampled for examination.
In cases where a prostate biopsy is performed, a Gleason score is assigned. Pathologists use this score to classify the grade of prostate cancer cells. It reflects how closely the abnormal cells resemble cancer and how aggressive their growth is.
- A Gleason score below 6 suggests that the cells do not show cancerous characteristics and carry a low risk.
- A Gleason score of 7 or higher, along with a PSA level between 10 and 20 nanograms per milliliter (ng/mL), indicates the presence of cancer cells that are likely not aggressive and grow slowly.
- A Gleason score of 8 or higher, along with a PSA level above 20 ng/mL, suggests a more advanced tumor.
- Imaging Tests: doctor may also prescribe imaging tests such as MRI, bone scans, or CT scans to evaluate the extent of cancer.
- Repeat PSA Testing: PSA blood tests monitor the level of prostate-specific antigen in the blood. Elevated PSA levels can be an indicator of prostate cancer, but there are many reasons for high PSA levels, leading to possible false-positive results.
Therefore, the Urology Society, unlike in the past, does not recommend the performance of the PSA test for prostate cancer screening. However, the PSA test is still suitable for specific cases, such as men at high risk of prostate cancer. Furthermore, if a prostate cancer diagnosis has previously been given, this test can assist in determining the stage or level of prostate cancer.

Prostate Cancer Treatment
Treatment options for prostate cancer depend on various factors, including the cancer’s rate of growth, extent of spread, overall health of the individual, and the advantages or side effects of the chosen treatment method.
In men with low-risk prostate cancer, immediate treatment may not be necessary. Some men may never require treatment. Instead, healthcare professionals sometimes recommend active surveillance.
In active surveillance, regular blood tests, planned examinations, anal examinations, and possibly biopsies can be conducted to monitor cancer progression. If these tests indicate cancer progression, an individual can choose a prostate cancer treatment method such as surgery or radiation therapy.
Active surveillance can be considered as a treatment option for cancer that does not produce symptoms, is expected to grow very slowly, and is confined to a small area of the prostate. Additionally, active surveillance may be an option for individuals who have other serious illnesses or are at an age where prostate cancer treatment may be challenging.
Prostate Surgery
- Prostatectomy
Prostate cancer surgery involves the removal of the prostate gland (radical prostatectomy), some surrounding tissues, and certain lymph nodes. Radical prostatectomy can be performed using several methods:
- Robotic-Assisted Surgery: During surgery with the assistance of a robot, instruments are connected to a mechanical device (robot) and inserted into the abdomen through several small incisions.
The surgeon sits behind a console (guidance device) and controls the robot’s movements using manual controls. Robotic prostatectomy enables the surgeon to perform more precise, minimally invasive surgical movements compared to traditional open surgery.
- Creation of an Incision in the Abdomen: In retropubic surgery, the prostate gland is removed through an incision made in the lower abdomen.
Orchidectomy (Testicle Removal)
Removing the testicles results in a reduction in the level of testosterone in the body.
Radiation Therapy
Radiation therapy utilizes high-energy radiation to target and eliminate cancerous cells. Prostate cancer radiation therapy can be administered in two ways:

- External Beam Radiation:
During external beam radiation therapy, the individual lies on a treatment table, and a machine surrounding their body delivers high-energy beams, such as protons and X-rays, to the prostate cancer. Typically, a person undergoes these external radiation sessions approximately 5 times a week for several weeks.
- Internal Radiation Seeds (Brachytherapy):
Brachytherapy involves placing numerous radioactive seeds into the prostate tissue, each about the size of a grain of rice. These radioactive seeds gradually release radiation over an extended period.
A physician uses a needle, guided by ultrasound imaging, to implant the radiation seeds into the patient’s prostate. These implanted seeds eventually exhaust their radioactivity, and there is no need for their removal.
Prostate Cancer Treatment
Hormone Therapy :
Hormone therapy is a treatment method aimed at halting the production of the male hormone testosterone by the body. Prostate cancer cells depend on testosterone for their growth. Suppressing testosterone production can either result in the death of cancer cells or slow down their growth. Hormone therapy options include the following:
Drugs that prevent testosterone from reaching cancer cells: Medications known as anti-androgens block testosterone from reaching cancer cells. Examples of these drugs include bicalutamide (Casodex), nilutamide (Nilandron), and flutamide. Enzalutamide (Xtandi) can be an option for hormone therapy when others are no longer effective.
Hormone therapy is used in men with advanced prostate cancer to shrink tumors and slow down tumor growth. In men with localized prostate cancer, hormone therapy can be used to shrink tumors before radiation therapy. This can increase the chances of success with radiation therapy.
Cryoablation of Prostate Tissue
Cryosurgery, or cryoablation, involves freezing tissue to eliminate cancer cells. During prostate cancer cryoablation, small needles are inserted into the prostate guided by ultrasound imaging. Extremely cold gas is circulated within the needles, causing the surrounding tissue to freeze.
Subsequently, secondary gas is used to thaw the tissue within the needles. This freezing and thawing cycle leads to the destruction of cancer cells and some surrounding healthy tissue.
Initial attempts to use cryosurgery for prostate cancer treatment resulted in unacceptable levels of complications and side effects. However, newer technologies have reduced complications, increased cancer control, and made the procedure more tolerable. Cryoablation is mostly used as a salvage therapy for men who have not responded to radiation therapy.
Chemotherapy
Chemotherapy employs drugs to target rapidly progressing cells, including cancer cells. Chemotherapy drugs can be administered intravenously, orally, or both. Chemotherapy can be an option for men whose prostate cancer has spread to distant parts of the body. Additionally, chemotherapy can be considered for cancers that do not respond to hormone therapy.
The treatment of prostate cancer is commonly carried out worldwide using two main methods: surgery and radiotherapy (brachytherapy and external beam radiation therapy).

Preventing Malignant Prostate Cancer
Malignant prostate cancer has certain uncontrollable risk factors such as age. However, other risk factors can be controlled. For instance, since research has shown that smoking increases the risk of developing prostate cancer, quitting smoking can reduce the risk of prostate cancer. Furthermore, diet and exercise are also significant factors that can influence the risk of prostate cancer.
Protecting the Prostate
Diet and Lifestyle:
Some certain foods can help reduce the risk of prostate cancer. Among these foods are:
- Tomatoes, cruciferous vegetables like broccoli, Brussels sprouts, and cabbage, and leafy greens.
- Fish, soy, and oils containing omega-3 fatty acids such as olive oil.
Some certain foods may increase the risk of prostate cancer. Among these foods are:
- Milk and dairy products.
- Saturated fats found in animal products.
- Red meat.
Exercising:
According to a study conducted in 2006 on 29,000 men, exercise can help reduce the risk of advanced prostate cancer and prostate cancer-related mortality.
Exercise can also assist in weight reduction, which is a key factor, as research has shown that obesity is a risk factor for prostate cancer. With your physician’s approval, aim for 30 minutes of exercise most days of the week.
The Last Word
In this article, we talked about the basics of prostate cancer, including its connection to age-related prostate gland changes. The causes, types, and prevalence of prostate cancer, considering factors such as genetics, lifestyle, and family history.
Also, we talked about the increasing risk with age and the significance of early detection.
This is where Dr. Maadico steps in. Early detection is key, and a consultation with Dr. Maadico’s Medical Department can provide you with personalized guidance.
Don’t let fear or misinformation hold you back. If you’ve experienced urinary issues, sexual dysfunction, or other symptoms, it’s crucial to address them promptly. Dr. Maadico’s Medical Department can guide you through the screening and diagnostic process with care and expertise.
Get a Free Consultation
FrAQ
- what is the cost of Prostate Cancer treatment?
The cost of treating Prostate Cancer varies a lot depending on factors such as the patient’s condition, the type of treatment, the stage of cancer, and the healthcare provider.
- What are the ways to prevent Prostate Cancer?
The likelihood of developing prostate cancer rises with age, and genetics also play a significant role. If your first-degree relatives (father, grandfather) have had prostate cancer, your risk increases. However, adhering to the following practices can help mitigate the risk of prostate cancer :
- Eating a healthy diet rich in fruits and vegetables
- Cutting down on fatty foods
- Having a regular exercise regimen
- Remaining physically active
- Maintaining a recommended weight
- Avoiding smoking and alcohol
- Is Prostate Cancer an inherited disease?
While there may be a genetic component to prostate cancer, it is not solely a genetic disease. Environmental factors and lifestyle also play crucial roles in the development of prostate cancer.
- How long is the hospitalization period for Prostate Cancer surgery?
The hospital stay for most prostate surgeries is around one to two days, and recovery at home is around four to six weeks. Consulting with the surgical team can provide specific information.

- What are the post-operative care procedures for Prostate Cancer?
Postoperative care methods for prostate cancer include:
- Regular movement shortly after surgery to prevent blood clots and other post-operative risks
- Pain control with over-the-counter medications.
- Catheter removal after the surgical site has healed, usually seven to ten days after surgery
- Avoiding vigorous activities or lifting heavy objects for at least one month after surgery.
- Regular follow-up appointments with the healthcare team
- What is the role of nutrition in Prostate Cancer development?
Good nutrition may reduce the incidence of prostate cancer and help reduce the risk of developing prostate cancer. A predominantly plant-based diet, with plenty of fruits and vegetables, high fiber, and low fat is recommended.
Some studies suggest that certain nutrients such as lycopene in tomatoes may have protective effects. However, individual nutritional needs can vary, and consultation with a nutritionist is recommended.
- Does alcohol, smoking, and addiction play a role in Prostate Cancer?
Numerous studies have investigated the correlation between alcohol consumption and prostate cancer. Some research suggests that past drinking habits may serve as a more reliable indicator of risk than current alcohol use.
On the contrary, other studies assert that heavy or ongoing heavy drinking elevates the likelihood of developing prostate cancer. Smoking, which can heighten levels of toxic inflammation, is also associated with more aggressive forms of prostate cancer.
Since prostate tumors typically exhibit slow growth, considering the history of alcohol consumption is important. In general, a high intake of alcohol is directly linked to the growth rate of tumors and the lethality of prostate cancer.
It is essential, however, to consider other factors that can influence the risk of prostate cancer in men. These factors include a history of high sexual activity, particularly at a young age, the presence of sexually transmitted infections, and unhealthy lifestyle .


